Abstract
Introduction: Hairy cell leukemia (HCL) is an indolent B-cell lymphoproliferative disease. BRAF V600E mutation is detected in nearly all classical HCL cases which offers the possibility of targeted therapy.
Objective: The aim of our study was to assess the efficacy of low-dose vemurafenib as well as to assess the long term outcome of HCL patients treated with this drug at the Department of Internal Medicine and Oncology at Semmelweis University.
Methods: We report on 10 patients with classical HCL treated with low-dose vemurafenib at our Department between 2013 and 2022.
Results: As a result of fixed time low-dose vemurafenib treatment, 5 of 10 patients (5/10) achieved partial remission, 4 (4/10) had stable disease, and 1 (1/10) had MRD positivity. No patients achieved complete remission. The median progression-free survival was 28.5 months while the overall survival was 82 months.
Conclusion: We confirm that low dose of vemurafenib is effective and safe in the vast majority of patients with HCL. This small-molecule oral treatment allows to gain valuable time—months or even years—before further, usually parenteral treatment options have to be given or before previous treatment has to be repeated. There are also promising data supporting the combination of vemurafenib with other drugs for the treatment of HCL patients which could provide even further possibility to bridge treatment.
Introduction
Hairy cell leukemia (HCL) is an indolent B-cell lymphoproliferative disease characterized by pancytopenia, splenomegaly, and infiltration of bone marrow, liver, and spleen with mature B cells. HCL as a well-defined entity was recognized in 1958 by [1].
It is a rare neoplasm representing 2% of lymphoid leukemias [2]. Affected patients often have non-specific symptoms including weakness and fatigue, as well as symptoms related to cytopenias and splenomegaly. Infectious complications are common, due to both the underlying immunosuppression from cytopenias and myelosuppressive therapy. In peripheral smear, the hairy cells present as characteristic-appearing mononuclear cells which are typically large with circumferential hair-like cytoplasmic projections and a round nucleus [3].
Diagnosis of HCL is based on the presence of hairy cells in the blood or bone marrow (BM). Hairy cells express the following markers: CD11c, CD19, CD20, CD22, CD103, CD123, and CD25. Histological examination of a bone marrow biopsy specimen is used to assess bone marrow infiltration. This highlights the clinical importance of immunophenotypic analysis. A wide range of antibodies have been reported as useful markers including annexin-A1, DBA.44 (mouse monoclonal HSL antibody), TRAP (tartrate-resistant acid phosphatase), Tbet, HBME1 (Hector Battifora) and BRAF V600E mutation specific mouse monoclonal antibodies [4].
The V600E mutation of the BRAF gene was identified in 2011 by using whole exome sequencing of genomic DNA from purified leukemic cells of a HCL patient by [5]. The mutation replaces thymine with adenine in exon 15 of BRAF at the 1799th nucleotide position of the coding sequence. This results in an amino acid change from valine to glutamate at the 600th amino acid position of the protein sequence and leads to aberrant activation of the MEK-ERK pathway, resulting in increased cell proliferation and survival. BRAF V600E mutation is detected in nearly all classical HCL cases and offers the possibility of targeted therapy [5]. The diagnostic toolkit has been expanded since 2011 (and is increasingly important) to detect the presence of the BRAF V600E mutation. BRAF gene mutation is detected by sequence analysis or using the monoclonal mouse antibody VE1 [6].
The current gold standard first-line treatment of hairy cell leukemia is the administration of purine nucleoside analogs (cladribine or pentostatin) [7]. Thanks to purine nucleoside analogue (PNA) treatment, the life expectancy of patients today does not differ from the life expectancy of the average healthy population, but 40% still have a relapse [8, 9]. Treatment with anti-CD20 monoclonal antibody, rituximab, is used with high efficacy not only in refractory cases but also in low tumor burden patients unsuitable for purine nucleoside analogue therapy [10–12]. Since the vast majority of HCL patients carry the BRAF p.V600E mutation the use of vemurafenib, a BRAF inhibitor, that shows an unusual specificity for the p.V600E mutation has been suggested in individual patients as early as 2012. By now it is an accepted treatment modality in relapsed/refractory hairy cell leukaemia patients. Moreover, in clinical studies the first line use of rituximab combined with vemurafenib is under evaluation.
Methods and patients
We report the treatment characteristics and long-term outcomes of 10 classical HCL patients treated with vemurafenib between January of 2013 and December of 2022 at the 1st Department of Internal Medicine and Oncology, Semmelweis University. In our institution HCL patients were diagnosed and treated within the addressed 10 years. Early results of our vemurafenib treated patients have been published in our 2013 (these patients are marked as No. 1,2,3 in the current paper—same as in the 2013 publication) [3]. Over the past four decades in our center the majority of HCL patients have received first-line treatment with alfa interferon. If there were no contraindications to PNA treatment and after the improvement of the blood counts subcutaneous cladribine treatment followed. Since 2013 those elderly and frail patients who progressed despite treatment with alfa interferon have received second-line vemurafenib (Patients No. 7, 8 and 10 in the present paper). All the patients underwent dermatologic examination at baseline.
Clinical data and follow-up information were collected by regular follow-ups and chart review. Follow-ups and control visits were carried out during an active treatment biweekly, after the active treatment period monthly, and after 6 months of stable disease every 3 months. Responses were evaluated based on blood counts, bone marrow findings, and peripheral blood hairy cell count using standard criteria (Table 1).
TABLE 1
| Response | Criteria |
|---|---|
| CR | ANC> 1.5 G/L, Hgb> 11 g/L, Thr> 100 G/L, no organomegaly by physical examination, no hairy cells in peripheral blood and bone marrow |
| MRD negative CR | ANC> 1.5 G/L, Hgb> 11 g/L, Thr> 100 G/L, no organomegaly, no hairy cell detected in bone marrow by immunohistochemistry |
| PR | ANC> 1.5 G/L, Hgb> 11 g/L, Thr> 100 G/L, organomegaly decreases by> 50%, hairy cell in peripheral blood <5%, bone marrow infiltration decreases by <50% |
| SD | CR and PR criteria are not met. |
| PD | Decrease in cell numbers> 25%, increase in organomegaly by> 25% |
| Relapse | Morphological relapse: recurrence of hairy cells in peripheral blood and/or bone marrow |
| Haematological relapse: development of cytopenia involving at least one cell line |
Criteria for response to treatment.
Patient characteristics are summarized in Table 2. Median age at diagnosis was 50 years (range, 35–68), at initiation of vemurafenib treatment was 73 years (range, 41–87). Patients were heavily pretreated (median of 2 prior treatment lines; range, 1–4 lines; n = 10). All consecutive treatments were administered due to progression.
TABLE 2
| Patient | Age at dg | Prior treatment lines | Time until treatment(month) | Duration of vemurfenib treatment (day) | Dose of vemurafenib (mg/day) | Response | PFS(month) | OS(month) | Side effect | Treatment after vemurafenib |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | 40 | 2 (caldribine, interferon) | 12 | 58 | 2 × 240 | PR | 37 | 115 | — | Rituximab, Cladribine |
| 2. | 45 | 3 (interferon, cladribine, rituximab) | 180 | 14 | 2 × 240 | SD | 2 | 89 | arthralgia hyperbilirubinaemia | Pentostatin |
| 3. | 65 | 3 (interferon, cladribine, rituximab) | 96 | 110 | 2 × 240 | SD | 32 | 72 | toxicoderma, arthralgia | IFN |
| 4. | 72 | 1 (interferon) | 56 | 56 | 2 × 240 | PR | 32 | 32 | photosensitivity | IFN |
| 5. | 64 | 2 (interferon, rituximab) | 228 | 14 | 2 × 240 | PR | 49 | 49 | tumorlysis sy (grade 2) | - |
| 6. | 48 | 3 (interferon, cladribine, rituximab) | 72 | 91 | 2 × 240 | SD | 14 | 89 | photosensitivity, arthralgia | IFN |
| 7. | 80 | 1 (interferon) | 84 | 14 | 2 × 240 | SD | 25 | 24 | toxicoderma | IFN |
| 8. | 69 | 1 (interferon) | 96 | 56 | 2 × 240 | PR | 8 | 78 | atrophy of skin | Rituximab |
| 9. | 35 | 4 (interferon, cladribine, interferon, rituximab) | 216 | 47 | 2 × 480 for 28 days | PR | 5 | 86 | keratoacanthoma | Rituximab mono 4x |
| 2 × 720 until day 47 | ||||||||||
| 10. | 72 | 1 (interferon) | 2 | 180 | 2 × 480 | MRD | 97 | 97 | hyperkeratosis | — |
Data from our patients treated with vemurafenib.
Descriptive and comparative statistical methods were used to analyze the clinical data.
BRAF V600E mutation–specific immunohistochemistry
Immunohistochemistry was performed on formalin-fixed, paraffin-embedded (FFPE) tissue using a mutation-specific antibody to BRAF V600E protein (VE1 clone; ready-to-use dilution; Ventana Medical System, Tucson, AZ) in a Leica Bond-Max automated immunostainer (Leica Biosystems, Deer Park, IL). Three-μm thick sections mounted on adhesive glass slides were deparaffinized and subjected to heat-induced epitope retrieval (HIER) at pH 9 (using Bond ER Solution 2) for 30 min before incubation with pre-diluted BRAF V600E mutation-specific primary antibody for 40 min. The Bond Polymer Refine Detection Kit (DS9800 Leica Biosystems, Deer Park, IL) was used to visualize reactivity. Immunoreactions were completed by nuclear counterstaining with hematoxylin.
Molecular analysis for BRAF mutations
The mononuclear cell fraction of peripheral blood or bone marrow samples collected in EDTA containing collection tubes was separated by Ficoll gradient centrifugation. Cellular DNA was extracted using the MagCore Plus II Automated Nucleic Acid Extractor (RBC Bioscience Corporation, Taiwan). Isolated DNA samples were quantified using a Qubit 4 Fluorometer (Thermo Fisher Scientific, USA) and stored at 4°C. The extracted DNA was subjected to PCR amplification of a 91 bp region of the BRAF gene harboring codon V600 with a forward (TGAAGACCTCACAGTAAAAATAGG) and a biotin-conjugated reverse primer (TCCAGACAACTGTTCAAACTGAT) using the ABI-Veriti 96 Well Thermal Cycler (Thermo Fisher Scientific, Waltham, MA). The amplified sequence was subjected to pyrosequencing of codons 599 to 601 using PyroMark Q24 (Quiagen). Briefly, single-stranded DNA templates for were obtained with the assistance of the PyroMark Q24 Vacuum Prep Workstation (Qiagen) according to manufacturer’s instructions. The DNA template was incubated with the sequencing primer (5′-TGATTTTGGTCTAGCTACA-3′) on the PyroMark Q24 heat-block at 80°C–85°C for 2 min. Pyrosequencing was performed using the following dispensation order (CGATGATC) on the PyroMark Q24 system following the manufacturer’s guidelines. All sequencing results were confirmed by pathologist review.
Results
Median time from diagnosis to treatment was 90 months (range, 2–228 months). Vemurafenib dose of 240 mg twice daily was used in 8 patients. Further patients received 480 mg twice daily (n = 2). Nine patients continued at this dose, whereas dose was escalated in 1 patient number 9. In patient number 9 we tried to deepen the remission by escalating the dose of vemurafenib. Dose and duration of the vemurafenib treatment was escalated in patient number 10 due to concomitant M. tuberculosis infection which was diagnosed before starting vemurafenib treatment. Median duration of vemurafenib treatment in the whole patient cohort was 56 days (range, 14–180 days).
Tables 3, 4 contains data on organ involvement, bone marrow infiltration and blood counts before initiating and after completion of vemurafenib treatment in all of our patients. As a result of vemurafenib treatment, 5 of 10 patients (5/10) achieved partial remission. 4 (4/10) had stable disease, and 1 (1/10) had MRD positivity. Patient number 1 achieved MRD positive CR after 180 days of vemurafenib treatment, at his 6 months bone marrow biopsy histology 2.4% residual hairy cells were found. MRD negative complete remission was not achieved in any of the patients. Median progression-free survival (PFS; from start of vemurafenib treatment to retreatment or death) was 28.5 months. Median overall survival (OS; from start of vemurafenib treatment to the end of our retrospective analysis or death) was 82 months. Median overall survival from the diagnosis to the end of the study or death was 164.5 months. During this long follow-up time 7 of 10 patients are still alive.
TABLE 3
| Patients | Before vemurafenib treatment | ||||
|---|---|---|---|---|---|
| - | - | - | Blood cell counts | ||
| - | Bone marrow infiltration | Organ involvement | White blood cell (G/L) | Hemoglobin (g/L) | Platelet count (G/L) |
| 1. | 30% hairy cell | Hepatosplenomegaly | 0.8 | 110 | 109 |
| 2. | 80% hairy cell | Splenomegaly | 0.8 | 100 | 49 |
| 3. | 30%–40% hairy cell | — | 1.1 | 110 | 107 |
| 4. | 90% hairy cell | — | 2.82 | 105 | 191 |
| 5. | diffuse infiltration | — | 1.11 | 63 | 23 |
| 6. | 80% hairy cell | Splenomegaly | 2 | 147 | 71 |
| 7. | 60%–70% hairy cell | — | 11 | 75 | 44 |
| 8. | 80% hairy cell | Splenomegaly | 3.58 | 131 | 54 |
| 9. | 40% hairy cell | — | 2.47 | 129 | 90 |
| 10. | 40% hairy cell | — | 2.66 | 156 | 94 |
Data about the blood counts, bone marrow- and organ involvement in our patients before vemurafenib treatment.
TABLE 4
| Patients | After vemurafenib treatment | ||||||
|---|---|---|---|---|---|---|---|
| - | - | - | Blood cell counts | ||||
| - | Bone marrow infiltration | Organ involvement | White blood cell (G/L) | Hemoglobin (g/L) | Platelet count (G/L) | ||
| 1. | <10% hairy cell | Splenomegaly | 4 | 155 | 98 | ||
| 2. | no data | Splenomegaly | 1.21 | 111 | 77 | ||
| 3. | 40% hairy cell | — | 2.3 | 141 | 118 | ||
| 4. | 70% hairy cell | — | 4.38 | 126 | 172 | ||
| 5. | there is no data | — | 2.56 | 78 | 89 | ||
| 6. | 40% hairy cell | — | 3 | 159 | 112 | ||
| 7. | no data | — | 2.77 | 104 | 72 | ||
| 8. | 60% hairy cell | Splenomegaly | 4.37 | 150 | 65 | ||
| 9. | 20% hairy cell | — | 3 | 111 | 162 | ||
| 10. | 24% hairy cell | — | 2.61 | 151 | 132 | ||
Data about the blood counts, bone marrow- and organ involvement in our patients after vemurafenib treatment.
Figure 1 shows the effectivity of vemurafenib exemplified by a patient’s control bone marrow biopsy.
FIGURE 1
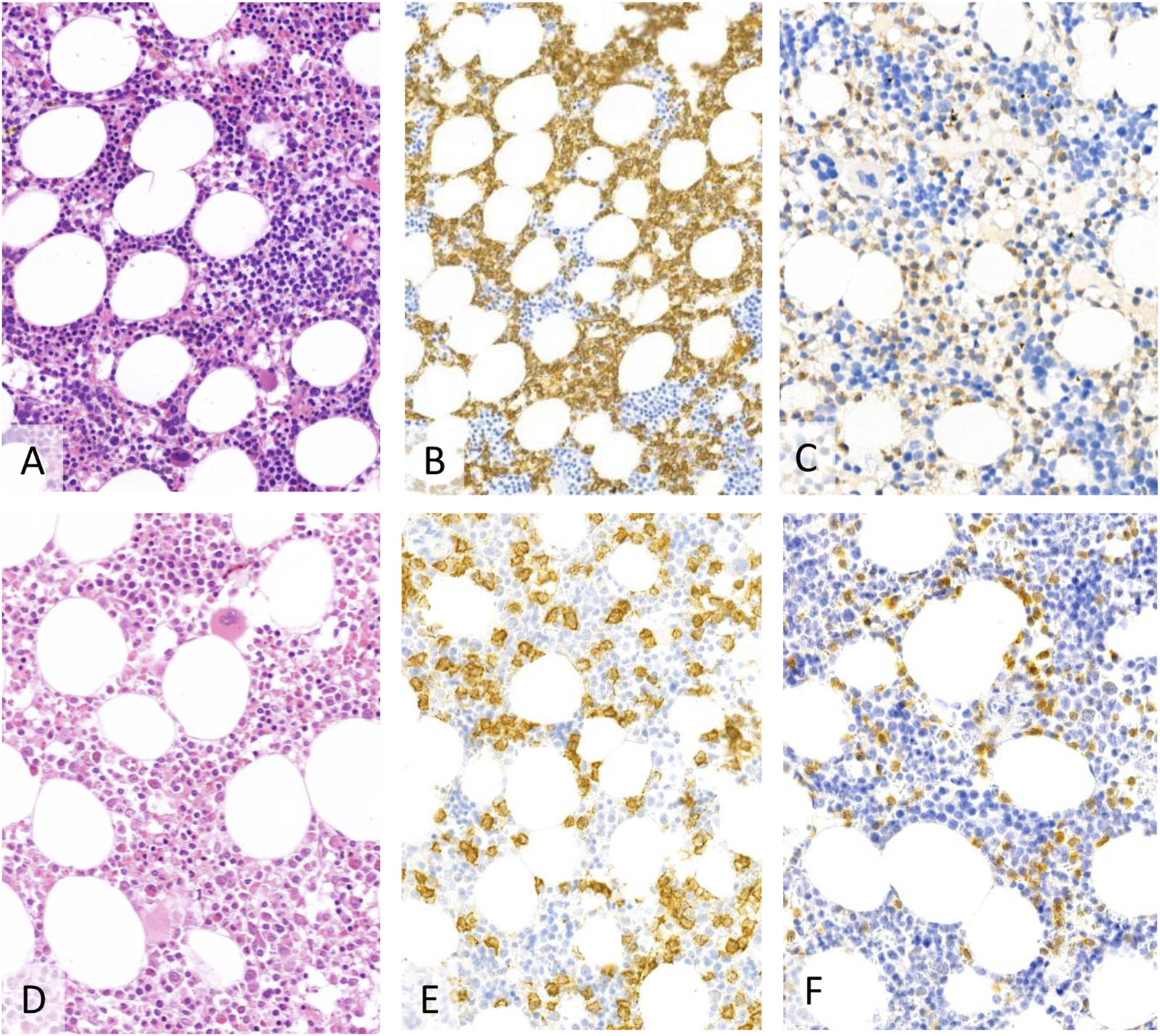
The first biopsy showed a more extensive infiltration (40%–50%) of hairy cell leukaemia ((A)–H&E, (B)–CD20, (C)–BRAF, 20X). After treatment the bone marrow was normocellular with maturing hematopoesis with residual patchy, interstitial lymphocytic aggregates ((D)–H&E) of CD20 positive (E) B-cells and with characteristic BRAF VE1 expression (F) accounting for ∼15%–20% of the cellularity.
To treat relapse following vemurafenib, 4 of 10 (4/10) patients received alpha interferon, 2 of 10 (2/10) patients received cladribine and rituximab, 1 of 10 patient (1/10) received rituximab, and 1 of 10 (1/10) received pentostatin. 2 patients did not receive treatment, because it was not necessary.
The side-effects of vemurafenib included photosensitivity (n = 2), toxicoderma (n = 2), keratoacanthoma (n = 1), hyperkeratosis (n = 1), arthralgia (n = 3), and elevation of bilirubin level (n = 1). In patient No. 5 grade 2 tumorlysis syndrome occurred as a side effect of the vemurafenib treatment within a few days. In patients with toxicoderma the skin symptoms disappeared after topical steroid treatment. Arthralgia was tolerable with non-steroidal agents. All patients were advised to stay out of the Sun. Side effects did not necessitate lowering of the dose or stopping the administration of vemurafenib.
Discussion
The discovery of the activating mutation BRAF V600E in 2011 has provided novel insights into the pathogenesis and had implications for the diagnosis and targeted therapy of HCL. This disease-defining genetic mutation, detected in nearly 100% of HCL patients, has opened the opportunity to investigate new targeted agents for the treatment of HCL [5]. The first reports documented in HCL patients treated with vemurafenib, a BRAF inhibitor approved for first-line treatment of unresectable or metastatic melanoma, been published in 2012 [13]. BRAF inhibitors such as vemurafenib are currently not approved in HCL and are used “off-label” in patients with refractory/relapsed HCL [14] In two phase 2 studies in 2015, that enrolled 54 BRAF-mutated HCL patients relapsed/refractory to purine analogue-based treatments, vemurafenib was administered at the standard melanoma dose of 960 mg twice daily for 16–18 weeks, respectively [15]. In comparison, patients in our study only received vemurafenib for an average of only 8 weeks. The ORR was 100% in the US study, 96% in the Italian study and the CR rate was 42% and 35%, respectively. MRD was detectable in all CR patients and relapses occurred soon after treatment. In our study no patient achieved complete remission with the shorter and lower dosing schedule. However, the median PFS in the Italian study was 9 months, which is significantly lower than the PFS we reported in the current analysis [15].
Dietrich et al. published a retrospective analysis of 21 refractory/relapsed HCL patients treated with vemurafenib at a lower dose (240 mg/day) with a median follow-up time of 17 months. The median duration of treatment was 90 days. The CR rate was 40%. Interestingly the median PFS (17 months) of these 21 R/R HCL patients is very similar to that found in our retrospective analysis (28.5 months), although our patients did not achieve complete remission [16].
Tiacci et al published the highly efficient and well-tolerated combination of vemurafenib + rituximab in refractory/relapsed HCL. Thus, new potential chemotherapy-free agents, the combination of BRAF inhibitors and anti-CD20 monoclonal antibodies may improve the duration of response and may add to the therapeutic armamentarium [17]. However, compared to this combination treatment, the advantage of vemurafenib monotherapy is that it can be used orally, requires less monitoring and adverse events are low-grade and manageable. Combined inhibition of BRAF and MEK represents another promising chemotherapy-free regimen that avoids infusion-related reactions, and infections potentially associated with rituximab treatment. There are also promising preclinical data with B cell lymphoma 2 (Bcl 2) inhibitor venetoclax, which support combinations with other drugs for the treatment of HCL patients [18].
Our results show that low dose of vemurafenib is effective and safe in the vast majority of HCL patients. Although none of our HCL patients achieved CR, still the overall survival of our R/R HCL patients is excellent. This indicates the very good therapeutic potential of vemurafenib to bridge the time between more aggressive therapies. Thanks to the lack of myelosuppressive and immunosuppressive effects, unlike PNA, vemurafenib is a chemotherapy-free option to treat HCL patients who have an active infection and who cannot wait for the infection to clear before starting treatment for HCL [19]. Thus, it could be administered even during the COVID-19 pandemic or in the event of an impending pandemic, either in the first-line setting or as a bridge to PNA until the resolution of the infection [20].
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by TUKEB Semmelweis University, Hungary. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
Conceptualization: CB, BT, and JD. Methodology: KF, BT, and JD. Resources, Clinical Care: KF, ZN, II, HE, and JD. Data Curation: KF and JD. Writing–Original Draft: KF. Writing–Review and Editing: ZN, II, BT, and JD. Visualization: CB and BT. Supervision: JD.
Acknowledgments
We thank the patients and their physicians for their participation in this research project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Bouroncle BA Wiseman BK Doan CA . Leukemic reticuloendotheliosis. Blood (1958) 13:164 609–30. 10.1182/blood.v13.7.609.609
2.
Sári E Rajnai H Dénes K Bödör C Csomor J Körösmezey G et al Novelties in the diagnostics and therapy of hairy cell leukemia. Új utak a hajas sejtes leukémia és a rokon kórképek diagnosztikájában és kezelésében. Magy Onkol (2016) 60:137–44. [Hungarian].
3.
Sári E Nagy ZG Baghy K Rajnai H Bödör C Csomor J et al Treatment of refractory hairy cell leukemia with a BRAF-inhibitor: lessons to be learnt. Pathol Oncol Res (2014) 20(4):973–80. 10.1007/s12253-014-9783-9
4.
Tóth-Lipták J Piukovics K Borbényi Z Demeter J Bagdi E Krenács L . A comprehensive immunophenotypic marker analysis of hairy cell leukemia in paraffin-embedded bone marrow trephine biopsies-a tissue microarray study. Pathol Oncol Res (2015) 21:203–11. 10.1007/s12253-014-9807-5
5.
Tiacci E Trifonov V Schiavoni G Holmes A Kern W Martelli MP et al BRAF mutations in hairy-cell leukemia. New Engl J Med (2011) 364(24):2305–15. 10.1056/NEJMoa1014209
6.
Andrulis M Penzel R Weichert W von Deimling A Capper D . Application of a BRAF V600E mutation-specific antibody for the diagnosis of hairy cell leukemia. Am J Surg Pathol (2012) 36(12):1796–800. 10.1097/PAS.0b013e3182549b50
7.
Maitre E Cornet E Troussard X . Hairy cell leukemia. 2020 update on diagnosis, risk stratification and treatment. Am J Hematol (2019) 94:1413–22. 10.1002/ajh.25653
8.
Saven A Burian C Koziol JA Piro LD . Long-term follow-up of patients with hairy cell leukemia after cladribine treatment. Blood (1998) 92:1918–26. 10.1182/blood.v92.6.1918.418k33_1918_1926
9.
Dinmohamed AG Posthuma EFM Visser O Kater AP Raymakers A Doorduijn JK et al Relative survival reaches a plateau in HCL. Blood (2018) 131:1380–8. 10.1182/blood-2017-12-820381
10.
Thomas Da O Brian S Bueso-Ramos C Fader S Michael J Francis J et al Rituximab in relapsed or refractory hairy cell leukemia. Blood (2003) 102:3906–11. 10.1182/blood-2003-02-0630
11.
Ravandi F O Brian S Jorgenden J Pierce S Faderl S Ferrajoli A et al Phase 2 study of cladribine followed by rituximab in patients with hairy cell leukemia. Blood (2011) 118:3818–23. 10.1182/blood-2011-04-351502
12.
Robak T Matutes E Catovsky D ESMO Guidelines Committee. Hairy cell leukaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol (2015) 5:100–7. 10.1093/annonc/mdv200
13.
Dietrich S Glimm H Andrulis M von Kalle C Ho AD Zenz T . BRAF inhibition in refractory hairy-cell leukemia. N Engl J Med (2012) 366:2038–40. 10.1056/NEJMc1202124
14.
Bohn JP Wanner D Steurer M . Ibrutinib for relapsed/refractory hairy cell leukemia variant. Leuk Lymphoma (2017) 58(5):1224–6. 10.1080/10428194.2016.1239262
15.
Tiacci E Park J De Carolis L Chung SS Broccoli A Scott S et al Targeting mutant BRAF in relapsed or refractory hairy-cell leukemia. N Engl J Med (2015) 373:1733–47. 10.1056/NEJMoa1506583
16.
Dietrich S Pircher A Endris V Peyrade F Wendtner CM Follows GA et al BRAF inhibition in hairy cell leukemia with low-dose vemurafenib. Blood (2016) 127(23):2847–55. 10.1182/blood-2015-11-680074
17.
Tiacci E De Carolis L Simonetti E Capponi M Ambrosetti A Lucia E et al Vemurafenib plus rituximab in refractory or relapsed hairy-cell leukemia. New Engl J Med (2021) 384(19):1810–23. 10.1056/NEJMoa2031298
18.
Vereertbrugghen A Colado A Gargiulo E Bezares RF Fernández Grecco H Cordini G et al In vitro sensitivity to venetoclax and microenvironment protection in hairy cell leukemia. Front Oncol (2021) 11(11):2595. 10.3389/fonc.2021.598319
19.
Bohn JP Pircher A Wanner D Vill D Foeger B Wolf D et al Low-dose vemurafenib in hairy cell leukemia patients with active infection. Am J Hematol (2019) 6:E180–2. 10.1002/ajh.25474
20.
Grever M Andritsos L Banerji V Barrientos JC Bhat S Blachly JS et al Hairy cell leukemia and COVID-19 adaptation of treatment guidelines. Leukemia (2021) 35(7):1864–72. 10.1038/s41375-021-01257-7
Summary
Keywords
relapsed/refractory, infection, hairy cell leukemia, BRAF inhibitors, vemurafenib
Citation
Ferenczi K, Nagy ZF, Istenes I, Eid H, Bödör C, Timár B and Demeter J (2023) Long term follow-up of refractory/relapsed hairy cell leukaemia patients treated with low-dose vemurafenib between 2013 and 2022 at the Department of Internal Medicine and Oncology, Semmelweis University. Pathol. Oncol. Res. 29:1611378. doi: 10.3389/pore.2023.1611378
Received
29 June 2023
Accepted
27 October 2023
Published
08 November 2023
Volume
29 - 2023
Edited by
Gábor Méhes, University of Debrecen, Hungary
Updates
Copyright
© 2023 Ferenczi, Nagy, Istenes, Eid, Bödör, Timár and Demeter.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Botond Timár, timar.botond@semmelweis.hu
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.